On Friday May 10 I attended a Patient Advocate seminar at the Nation Cancer Institute in Bethesda Maryland. The seminar was to train new patient advocate volunteers, who sit on committees or task forces and help review clinical trial proposals. I, along with two other experienced patient advocates, were invited to share our experiences. Throughout the day we old-timers chimed in with our thoughts, then we wrapped up the conference with a panel. I was the mop-up guy since the moderator had to leave early. It was a good experience to meet with a mentor the volunteers who had experienced cancers, either themselves or as a caregiver, and who were willing to help remind clinicians and researchers about the person on the pointy end of the needle.
The keynote presentation was by Dr. Stephanie Goff, a senior research physician in NCI's Center for Cancer Research. Her presentation was on immunotherapy for cancer, the when and the why. With Dr. Goff's permission, I am including her slide deck in this blog post. Her first four slides set the stage for using immunotherapy to treat cancer:
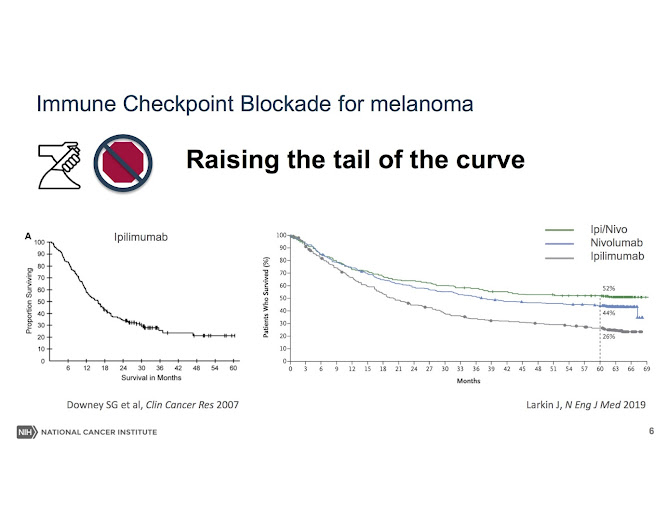
Dr. Goff's presentation focused on a subject that is of particular interest to me: how immunotherapy has increased "the tail of the curve" and helped raise the number of long-term survivors:
These charts, called Kaplan-Meier curves, graphically illustrate how long patients live after being diagnosed with various types of cancers. For example, when I was diagnosed in 2011, a Kaplan-Meier curve for metastatic bladder cancer patients between 2000-10 showed that 80% had died within two years, and 95% had died within 5 years. The chart ended at 6.5 years, suggesting that no one in that study had lived longer than that. I've learned that the focus of modern cancer research and treatment is to extend life -- to "raise the curve" -- instead of an audacious goal of "curing" everyone with one treatment.
Dr. Goff's presentation covered the development of immunotherapy therapies:
I was astonished to hear Dr. Goff explain that there was reported data for certain cancers that had been treated with immunotherapy which showed that there is a subgroup of patients who have been treated with immunotherapy and have experienced "durable life-long regression of metastatic cancer" (slide 9):
That conclusion -- "immunotherapy can mediate durable life-long regression of metastatic cancer" -- is as close as a skilled researcher will get to the loaded "c" word: cure. Researchers do not like to speak of a cure for cancer, because "cure" is a loaded word, maddeningly vague and weighted with hope to laypersons. Instead, they speak of "progression-free survival" (PFS) and "no evidence of disease" (NED). I've learned to avoid using the "c" word and to orient my thinking around the durability of my remission. And as I approach the fourth anniversary of my fourth and current remission, I continue to nurse a hope that maybe, just maybe, this one will in fact be durable.
Dr. Goff's presentation reinforced an emerging acceptance of the fact that I might not soon die from cancer. For 12 years I've stood on the precipice of death, with scans every 12 weeks to assess whether my mets have returned. On four different occasions those scans have revealed new metastatic activity: first in April 2012, second in September 2013, third in August 2014, and fourth in February 2017. I'm now four years into my fourth remission, and gradually am accepting that I might, just maybe, live a bit longer than I've expected. But still I doubt.
The next dozen of of Dr. Goff's slides illustrate when immunotherapy is indicated, and provides examples from several types of cancers of immunotherapy successes. (slides 10-21)
Dr. Goff closed with a caution of how much we still don't know: while immunotherapy can have a durable benefit (still avoiding the "cure" word), we don't have sufficient predictive tools of whether immunotherapy will work on any specific patient. The biomarkers from genetic sequencing of tumors are not consistently predictive or whether immunotherapy will work. Likewise, biomarkers do not predict which which patients will suffer which adverse side effects. In addition, new immunotherapy drugs are being approve not based upon overall survival (OS), which is the best data for drug approval, but instead upon progression-free survival (PFS) or relapse-free survival (RFS). True, these drugs show a promising capacity to extend life, but more time is needed to give definitive proof. But this class of drugs shows great promise, and without a doubt has saved my life.Dr. Goff's conclusion was that checkpoint blockage immunotherapy, like the Nivolumab therapy that I've had, is "more likely to lead to a long duration response than chemotherapy":
























No comments:
Post a Comment
Spam comments will not be accepted for posting.